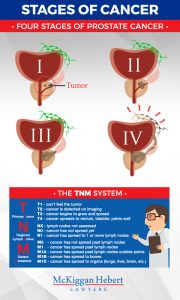
It’s scary to hear the words, “You have cancer.” But the distress and concern of worrying about your health can be compounded by the realization that the diagnosis was delayed, allowing the cancer to grow and spread.
A delayed cancer diagnosis can give rise to a medical malpractice claim. This type of claim, however, faces many challenges that malpractice lawyers and their clients should be aware of.
Many Canadians will face a cancer diagnosis at some point
The Canadian Cancer Society reports that 2 of 5 Canadians will develop cancer in their lifetime, and that 1 of 4 will die from cancer. Since the 5-year survival rate of someone with cancer is about 63% (it varies according to the type of cancer) a missed or delayed diagnosis means that a patient may have missed a lifesaving opportunity for treatment.
Earlier Diagnosis = Better Results
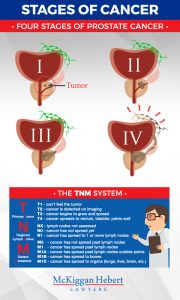 Generally speaking, if one is diagnosed early, there is a greater chance of survival. But, what if a medical practitioner acts negligently in determining the health of a patient? There may be grounds for a medical malpractice claim if a doctor’s unreasonable delays in diagnosing cancer mean the patient loses the opportunity for effective medical care.
Generally speaking, if one is diagnosed early, there is a greater chance of survival. But, what if a medical practitioner acts negligently in determining the health of a patient? There may be grounds for a medical malpractice claim if a doctor’s unreasonable delays in diagnosing cancer mean the patient loses the opportunity for effective medical care.
You Cannot Sue for “Loss of Chance” in Canada
Medical malpractice claims relating to a delayed diagnosis face many hurdles in Canada. Americans plaintiffs can try to show that a physician’s delayed diagnosis reduced their chances for successful treatments, by some percentage. Say a plaintiff in the U.S. claims that a delayed diagnosis reduced the chance of successful treatment by 20%. The plaintiff, then, can try to sue for 20% of potential future losses. This is called “loss of chance”. You cannot sue a medical practitioner for “loss of chance” like one could in the United States.
Burden of Proof in Cancer Claims
A plaintiff in Canada must show more than just a possible loss of chance. Plaintiffs in this country have to prove, on the balance of probabilities, that an earlier diagnosis would have changed the outcome of treatment. Meaning that they would likely not have experienced the loss had they been diagnosed earlier.
While difficult to prove, there are several ways plaintiffs and their medical malpractice lawyers can show that a missed or delayed diagnosis caused enough harm to win damages in a cancer misdiagnosis case.
Showing Causation
Cancer misdiagnosis claims in Canada must begin with the plaintiff proving causation, which means certain circumstances need to be established, on the balance of probabilities, through examination of legal and medical issues. These circumstances include:
Continue reading →